Helping healthcare providers manage submitting and processing medical insurance claims
Brief Understanding of What a Medical Claims Management System Is
A medical claims management workflow system is a software system that automates the claims management process and provides a platform for healthcare providers and 3rd party insurance companies to manage their claims efficiently, accurately & securely.
Designed to meet the needs of 3rd party ancillary medical management solutions for the workers’ compensation businesses, this software offers a comprehensive solution for medical claims capture, workflow, approval, archive, retrieval and sharing. With its intuitive interface and advanced features, it streamlines document management processes and saves users time and effort.
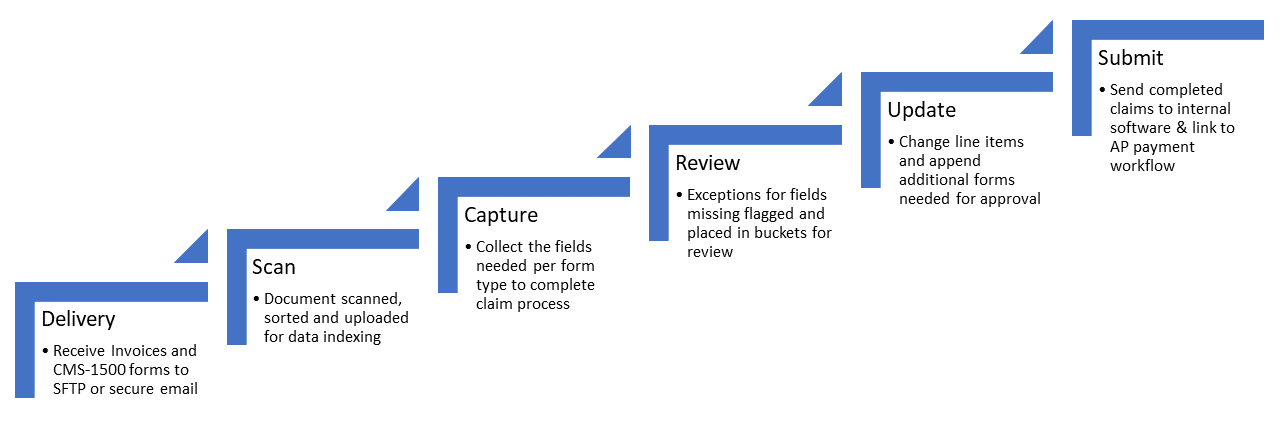
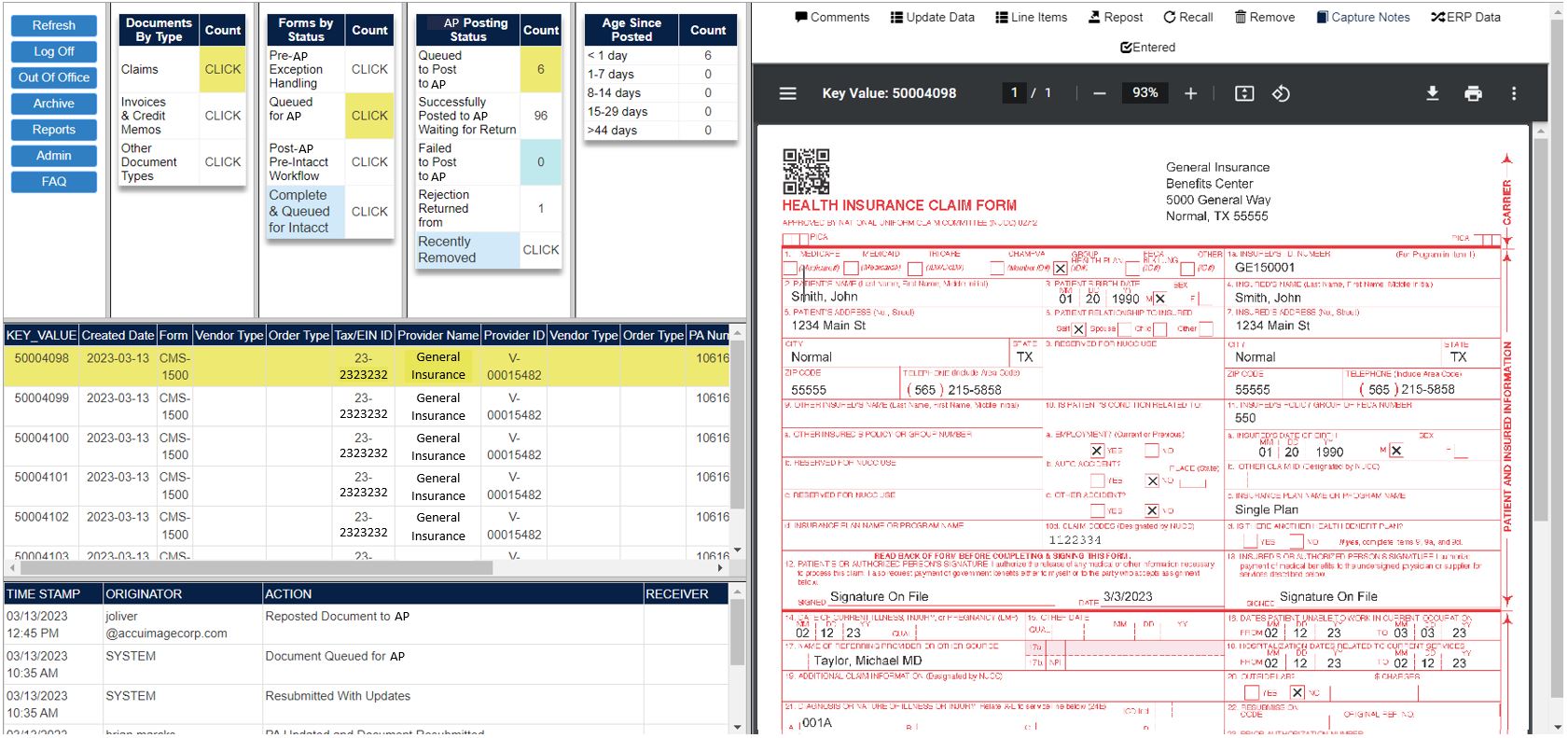
The AccuImage MCM workflow tool gives users the ability to manage CMS1500 forms and the exceptions that come with them. Most times these forms are submitted incomplete and the efforts to discover what is needed take time and effort from the ancillary medical claims management team. With AccuImage efforts to load all fields into this workflow, missing fields can be easily identified and sorted into the correct buckets for corrective action.
Different user types are created so managers may see all parts of the workflow, and restrict access for processors to have a clear path to work through the claims. If claims sit too long in a bucket, before reaching a deadline that may be missed, a notification can be sent to managers to alert them for potential claims being passed over.
The invoices that are associated with the CMS1500 claims are tracked right in the workflow as well, for a clear view of the status of every claim being processed. Invoices can be handled by the AccuImage Accounts Payable Automation solution, or by connecting to existing AP workflows / ERP systems. Connections to Payment Portals also allow for the entire process to be handled in one location.
Full history of all actions taken on all documents, as well as customized detailed business intelligence reporting, allow for full insight into each claim. The free included archive and retrieval tool makes audits easier than ever with the ability to search on any field that has been captured.
Documents are organized into buckets by their type & status. Metadata can be utilized for quick and efficient search
Management can view documents status and generate reports on-demand regarding workloads and throughput
User access is managed by levels of permissions, ensuring that sensitive data is only accessible those authorized
Software integrates with email, ERPs, CRMs & payment providers to simplify workflows & increase productivity
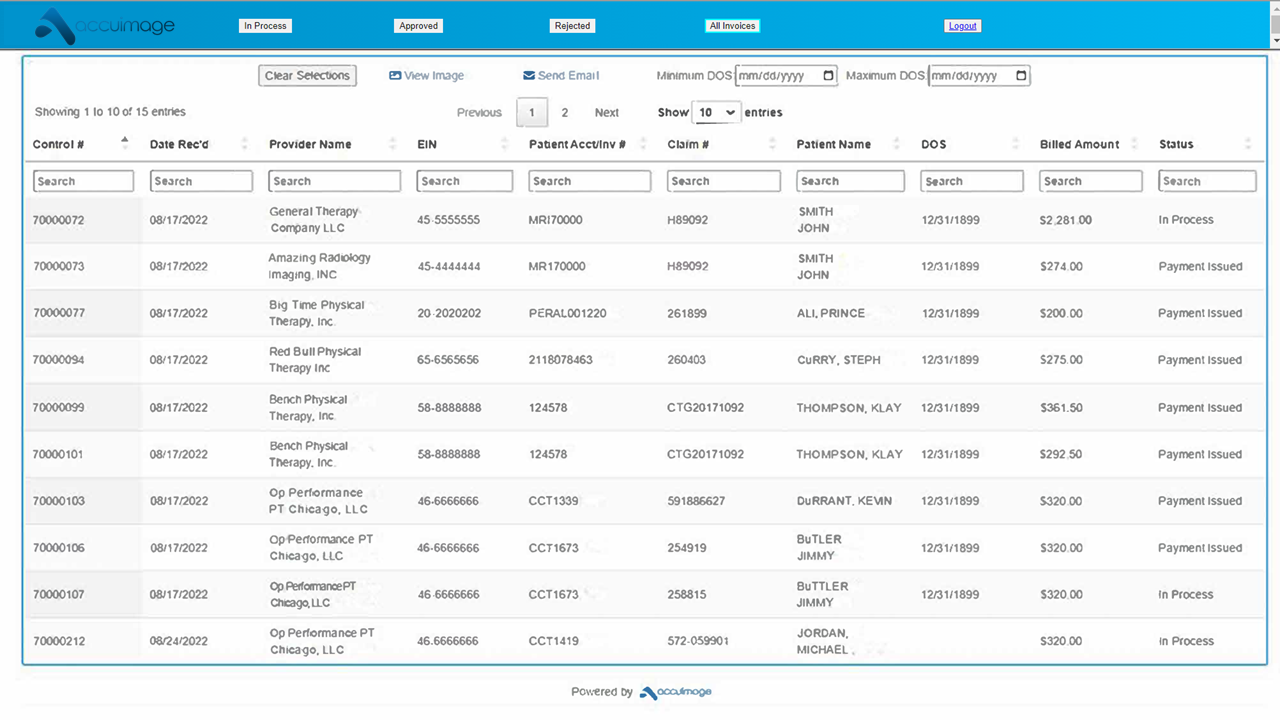
This feature gives providers an interactive ability to see an entire cross section of current and past transactions, in multiple statuses. With this ability, communication the Provider looking for additional details can be greatly reduced with less emails & phone calls inquiring about status of invoices. This tool also gives internal staff ability to monitor and manage Providers proactively rather than reactively with reporting and alerts.
Top 5 largest 3rd party ancillary medical management companies implemented the AccuImage MCM system
Labor Hours Decreased
Time Per Claim Decreased
Claim Denials Decreased
Claims that have exceptions are no longer rejected immediately and are instead processed using an exceptions bucket with tools to help remedy the line item errors
The indexing team captures the info off documents and routes claims to the right bucket, flagging what is missing, and giving users tools to add in the correct data
Setup custom rules for multiple payers for insurance companies and government programs to reduce the complexity of the claim process and reduce manual steps
Status monitoring of all claims processing & customized reporting allows for visibility to no longer cause claims to be rejected due to timeliness with alerts set to meet deadlines
AccuImage is HIPAA compliant and SSAE 16 Type II certified to keep all data encrypted at rest and in motion through the workflow steps
Words from AccuImage Development Team
"We are excited to offer our customers this powerful tool for managing their claims. With the growing volume of hardcopy, soft copy and EDI claims that ancillary medical management companies need to manage, we believe that our software will help companies save time, increase efficiency, and improve their bottom line."
To arrange a demonstration or more information, send us a message.
